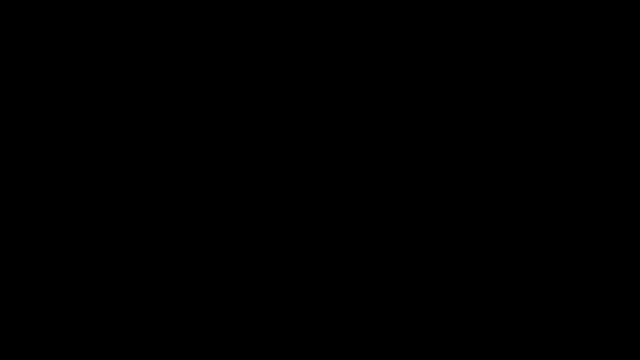
I’m not just a lockdown sceptic. I know lockdowns increase infections rather than decrease them because I read research first hand. I’m a citizen in a democracy who wants Government policy to be evidence-based, not epidemiological modelling based. Crazy, I know.
https://t.co/FokkJhgtzM
https://t.co/TPRYQ1LAAJ
https://t.co/99FR4IqbJj
https://t.co/5N06jgA0Bg
https://t.co/gX6xuQz5EY
https://t.co/0FwTjxpKtR
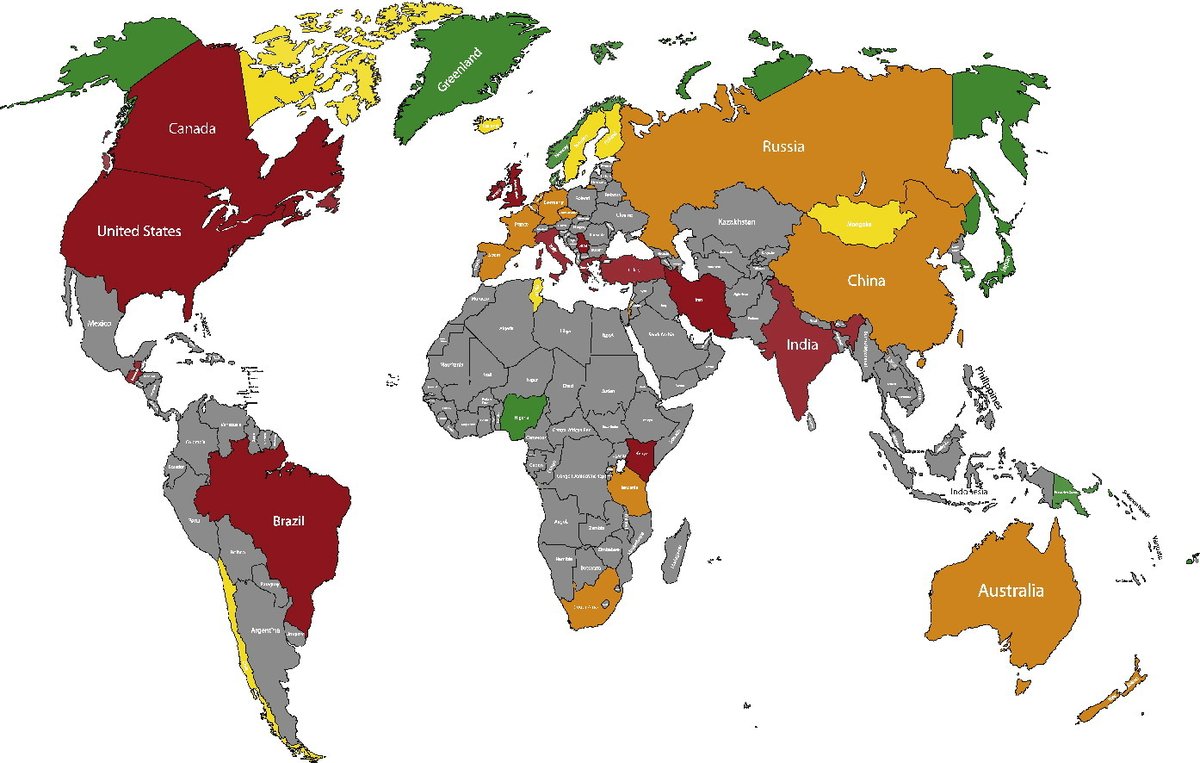
Green=High Omega-3 levels
Red=Low Omega-3 levels
https://t.co/h0HzV1Y5gN
https://t.co/vAw4pphsSC
https://t.co/RPagpdYkll
"Technically speaking, inflammation occurs when the amount of omega-6 fatty acids you consume outweigh the\xa0omega-3 fatty acids. Omega-6s are an essential part of a healthful diet, but they\u2019re also the primary building blocks of pro-inflammatory hormones."https://t.co/bK37z3VMae
— Robin Monotti (@robinmonotti) December 19, 2020
https://t.co/2STxtMHVmA
More from Robin Monotti
I have now re-examined this document:
It clearly does indicate both the risks of bacterial infection & to prescribe broad spectrum antibiotics as part of treatment:
"Collect blood cultures for bacteria that cause pneumonia and sepsis, ideally before antimicrobial therapy. DO NOT
delay antimicrobial therapy"
"6. Management of severe COVID-19: treatment of co-infections
Give empiric antimicrobials [broad spectrum antibiotics] to treat all likely pathogens causing SARI and sepsis as soon as possible, within 1 hour
of initial assessment for patients with sepsis."
"Empiric antibiotic treatment should be based on the clinical diagnosis (community-acquired
pneumonia, health care-associated pneumonia [if infection was acquired in health care setting] or sepsis), local epidemiology &
susceptibility data, and national treatment guidelines"
"When there is ongoing local circulation of seasonal influenza, empiric therapy with a neuraminidase inhibitor [anti-viral influenza drugs] should
be considered for the treatment for patients with influenza or at risk for severe disease."
On the 19th March 2020 the WHO released this guidance intended for healthcare workers (HCWs), healthcare managers and IPC teams at the facility level & at national and district/provincial level:https://t.co/C4aV2BnMPj pic.twitter.com/tCk1EyLskV
— Robin Monotti (@robinmonotti) December 21, 2020
It clearly does indicate both the risks of bacterial infection & to prescribe broad spectrum antibiotics as part of treatment:
"Collect blood cultures for bacteria that cause pneumonia and sepsis, ideally before antimicrobial therapy. DO NOT
delay antimicrobial therapy"
"6. Management of severe COVID-19: treatment of co-infections
Give empiric antimicrobials [broad spectrum antibiotics] to treat all likely pathogens causing SARI and sepsis as soon as possible, within 1 hour
of initial assessment for patients with sepsis."
"Empiric antibiotic treatment should be based on the clinical diagnosis (community-acquired
pneumonia, health care-associated pneumonia [if infection was acquired in health care setting] or sepsis), local epidemiology &
susceptibility data, and national treatment guidelines"
"When there is ongoing local circulation of seasonal influenza, empiric therapy with a neuraminidase inhibitor [anti-viral influenza drugs] should
be considered for the treatment for patients with influenza or at risk for severe disease."
You May Also Like
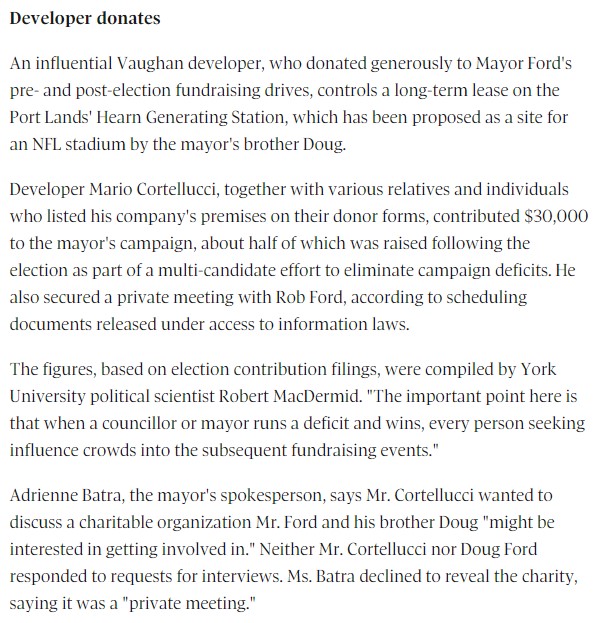
fascinated by this man, mario cortellucci, and his outsized influence on ontario and GTA politics. cortellucci, who lives in vaughan and ran as a far-right candidate for the italian senate back in 2018 - is a major ford donor...

his name might sound familiar because the new cortellucci vaughan hospital at mackenzie health, the one doug ford has been touting lately as a covid-centric facility, is named after him and his family
but his name also pops up in a LOT of other ford projects. for instance - he controls the long term lease on big parts of toronto's portlands... where doug ford once proposed building an nfl stadium and monorail... https://t.co/weOMJ51bVF
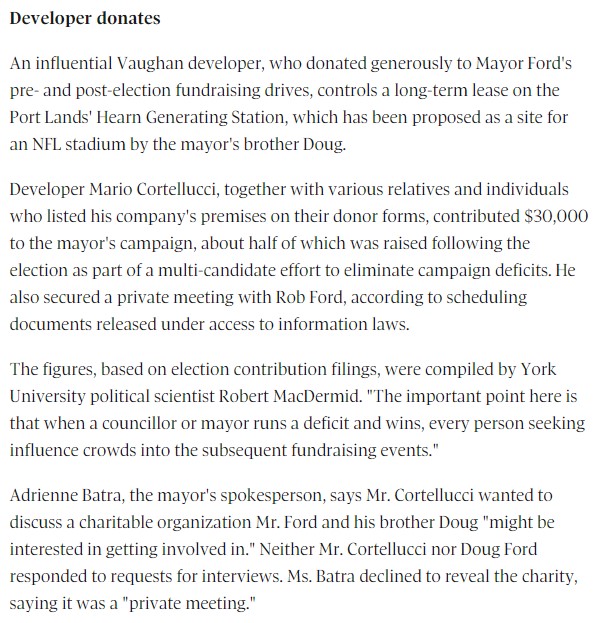
cortellucci, who is a developer, also owns a large chunk of the greenbelt. doug ford's desire to develop the greenbelt has been
and late last year he rolled back the mandate of conservation authorities there, prompting the resignations of several members of the greenbelt advisory

his name might sound familiar because the new cortellucci vaughan hospital at mackenzie health, the one doug ford has been touting lately as a covid-centric facility, is named after him and his family
but his name also pops up in a LOT of other ford projects. for instance - he controls the long term lease on big parts of toronto's portlands... where doug ford once proposed building an nfl stadium and monorail... https://t.co/weOMJ51bVF
cortellucci, who is a developer, also owns a large chunk of the greenbelt. doug ford's desire to develop the greenbelt has been
and late last year he rolled back the mandate of conservation authorities there, prompting the resignations of several members of the greenbelt advisory