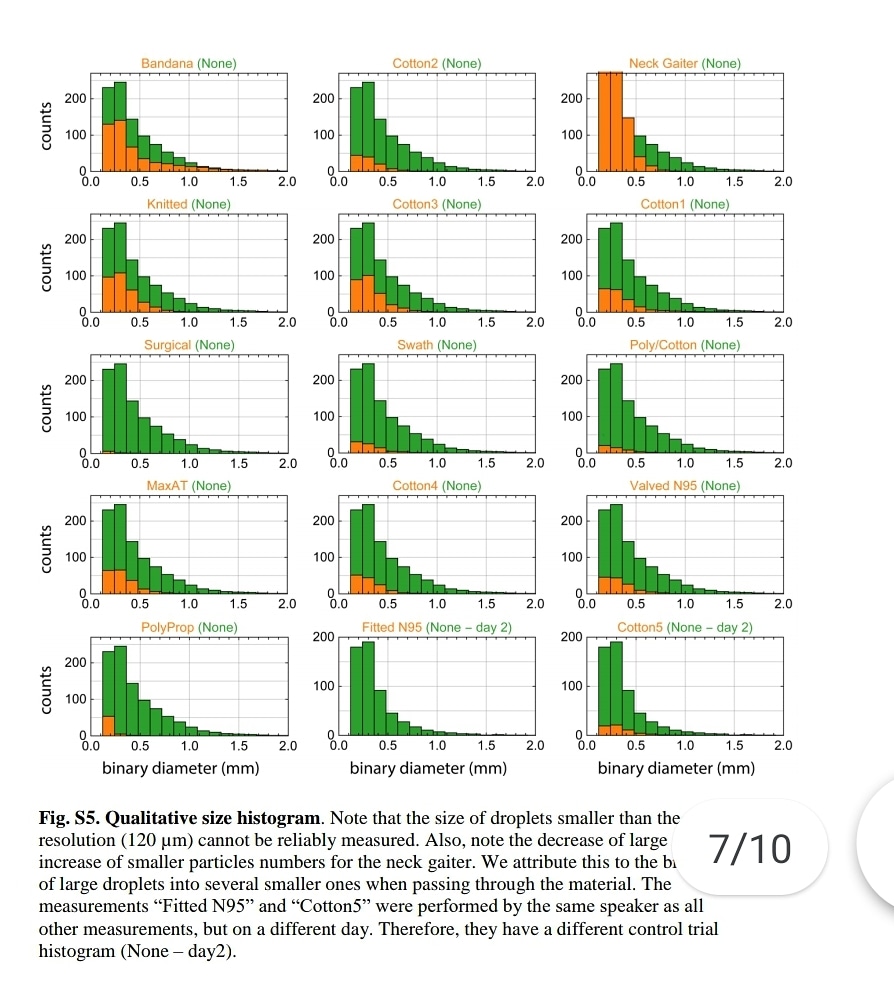
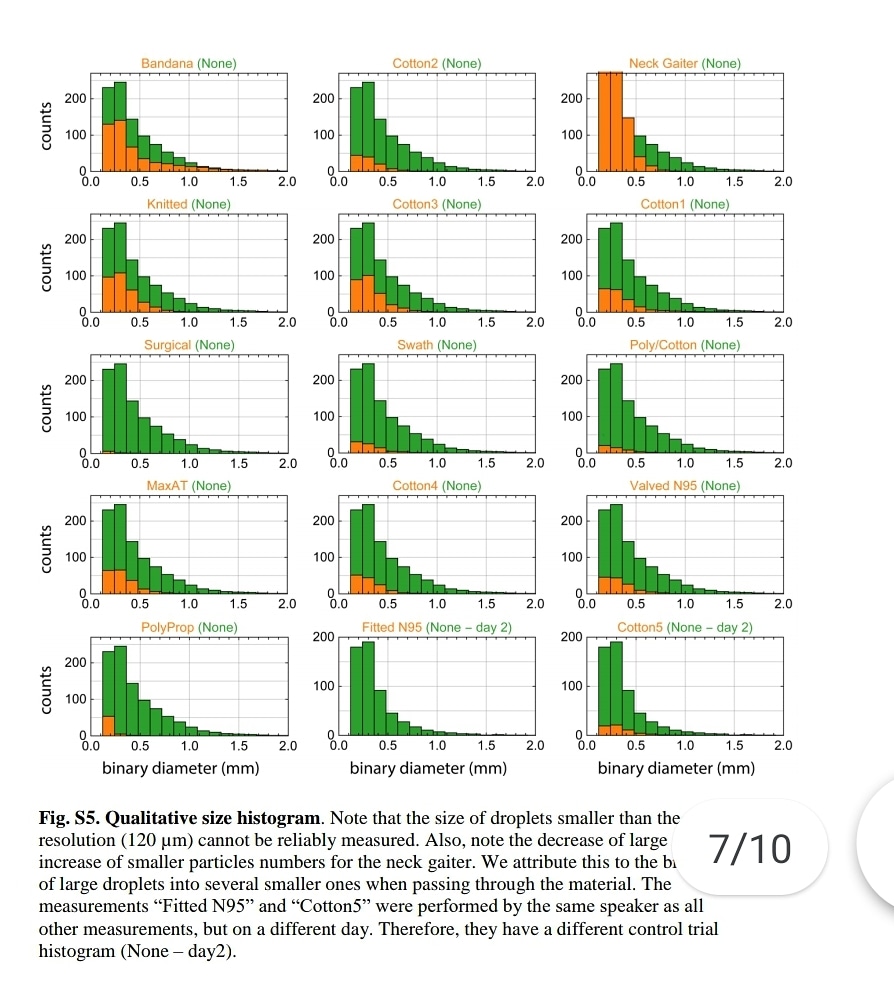
"Speaking through some masks dispersed largest droplets into a multitude of smaller droplets..smaller particles are airborne longer than large droplets (larger droplets sink faster), a mask might be counterproductive."
https://t.co/jBQlWRxcEL
Influenza like illness rates 3 times higher with cloth masks when compared to control group:
https://t.co/djT0mfutv9 Prof. Carl Heneghan, Oxford University: "The high quality trial evidence for cloth masks suggest they increase your rate of reinfection."
Please note, droplets smaller than 120 microns can't be measured. SARSCoV2 is 0.14 microns. This means that the nebulization effect of medical masks could not be measured, not that it does not happen. ⬇️
https://t.co/uAmlclH2jQ
The really small aerosols <1 μm [the ones that pass through ALL surgical masks] can penetrate all the way to the alveoli - the basic units for gas exchange ⬇️
https://t.co/BxVILCjtM0
Why does nebulization (the breaking up of larger aerosols which fall quicker into smaller ones which float for longer) cause more severe cases & deaths? Explained in this thread:
https://t.co/icOmr0advF
So although medical masks filter out coarse aerosol particles (which stay on the mask only to either later evaporate into smaller ones or be re-inhaled or re-exhaled), it is the finer smaller aerosols which are most conducive to transmission of severe disease on all counts.
"Fine particles contained 8.8 fold more viral copies than did coarse particles." This accounts for fine sized particles which can be measured, finer particles than those in this study (those which contain SARSCoV2) can't actually be measured reliably.
https://t.co/A6YBcGZLVN
In conclusion, the nebulization effect into the smallest aerosols which has been measured reliably for all non medical masks, & assumed to be happening for medical masks too, increases both transmission & severity of disease for a number of different reasons:
1 Masks break up larger aerosols into smaller aerosols: the nebulization effect
2 Smaller particles float in air for longest, larger particles drop
3 Smaller particles get deeper into the lungs, leading to more severe infection & higher mortality
4 Reduce oxygen & increase CO2
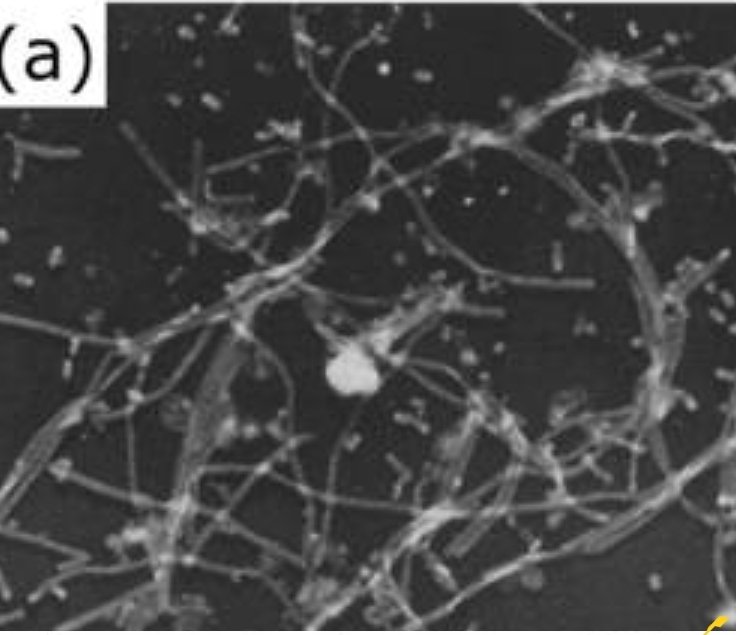
The smallest aerosols which float in air for longest & contain most virions can directly reach the alveolar region in the lungs & attack alveolar cells that produce Pulmonary Surfactant which is needed to lower surface tension & prevent alveoli collapse:
https://t.co/77i7BWcpwF
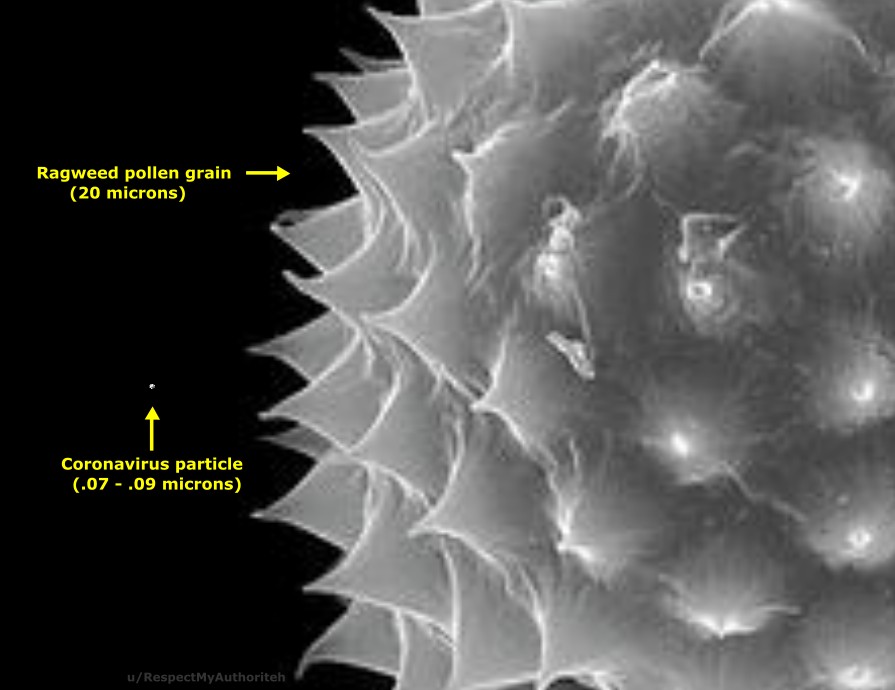
This is why the Japanese started wearing face masks in Spring-Summer: pollen related hayfever & pollution. Look at the difference in size of a pollen with a coronavirus particle.
When science was scientific:2003: "N95 Masks Flying Off Shelves, but They Offer Scant Protection: Bad fits are deadly. Contaminated air breathed from around the unfiltered edges instead of through the N95-rated material undermines the purpose of a mask."
https://t.co/gDUiS1Ujet
Contrary to SARSCoV2, the length of influenza particles varies considerably, influenza is pleomorphic, the size can be in excess of many tens of micrometers, producing filamentous virions reaching or exceeding 30 μm in length:
https://t.co/lLvsmtGUmb
This means that randomised controlled trials for medical masks for the spread of the influenza virus may have different results than RCTs for the SARSCoV2 virus, which really leaves us with a single RCT on the use of medical masks (N98s with instructions on use) in the community:
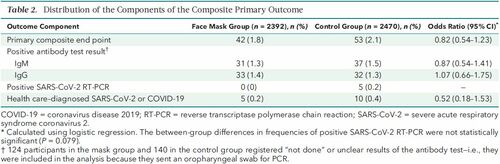
Unlike other studies looking at masks, Danmask was a randomised controlled trial – the highest quality scientific evidence. It revealed a minimal statistical difference between those who wore medical masks & those who did not in terms of COVID-19 infection
https://t.co/WRFEAEE5wW
⬆️ This was written by a Professor of Evidence-Based Medicine, Director of the Centre for Evidence-Based Medicine & Director of Studies for the Evidence-Based Health Care Programme & Centre for Evidence-Based Medicine, University of Oxford, with a senior tutor & research fellow.
Danmask (original below) proves N98 masks make no difference to the user on whether they get infected. Contrary to popular unscientific belief, I demonstrate above that non medical masks worn by a SARSCoV2 infected person increase transmission to others compared to no mask use.
DANMASK RCT for N98 masks: (SARSCoV2 prevalence was 2%)
People who got infected:
1.8% in the mask group
2% in group who wore masks exactly as instructed
2.1% in the no mask group:
"The difference observed was not statistically significant."
https://t.co/rCtekH6eoT
DANMASK: "In this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon and was not among other recommended public health measures related to COVID-19,
>>
<< a recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, incident SARS-CoV-2 infection compared with no mask recommendation."
Droplets vs Aerosols:
"Droplets are larger (>5 μm) rapidly drop to the ground by force of gravity.
Aerosols are smaller (≤5 μm) rapidly evaporate, leaving behind droplet nuclei that are small enough & light enough to remain suspended in the air for hours (analogous to pollen)."
"If SARS-CoV-2 is primarily spread by respiratory droplets, wearing a medical mask, face shield, or keeping 6 feet apart from other individuals should be adequate to prevent transmission." [DANMASK proved SARSCoV2 is not primarily spread by droplets].
"If, however, SARS-CoV-2 is carried by aerosols that can remain suspended in the air for prolonged periods, medical masks would be inadequate (because aerosols can both penetrate and circumnavigate masks) >>
<< face shields would provide only partial protection (because there are open gaps between the shield and the wearer’s face), and 6 feet of separation would not provide protection from aerosols that remain suspended in the air or are carried by currents."
"Experimental data support the possibility that SARS-CoV-2 may be transmitted by aerosols (so-called airborne transmission) even in the absence of aerosol-generating procedures" [even in the absence of the further aerosol nebulization provided by breathing through face masks].
"Speaking & coughing produce both droplets & aerosols..it is feasible for SARS-CoV-2 to remain suspended in the air & viable for hours, SARS-CoV-2 RNA can be recovered from air samples in hospitals, poor ventilation prolongs the amount of time that aerosols remain airborne."
"Demonstrating that speaking and coughing can generate aerosols or that it is possible to recover viral RNA from air does not prove aerosol-based transmission; infection depends as well on the route of exposure, the size of inoculum, the duration of exposure, and host defenses."
"Close but less sustained contact such as sharing a meal is associated with a secondary attack rate of about 7%, whereas passing interactions among people shopping is associated with a secondary attack rate of 0.6%."
"Prolonged exposure to an infected person in a poorly ventilated space..allows otherwise insignificant amounts of virus-laden aerosols to accumulate."
Therefore the aerosol mode of transmission may not be the only one, but it is the one which leads to the most severe disease & higher mortality as it reaches deeper into the lungs. Ventilation, not face masks, is the solution:
https://t.co/eHbaBbaPtk
When it comes to respiratory diseases, a healthy person is someone who has no symptoms of a respiratory disease. Chemical reactions in man made objects do not change this. Thread:
https://t.co/7VSaerYh5p