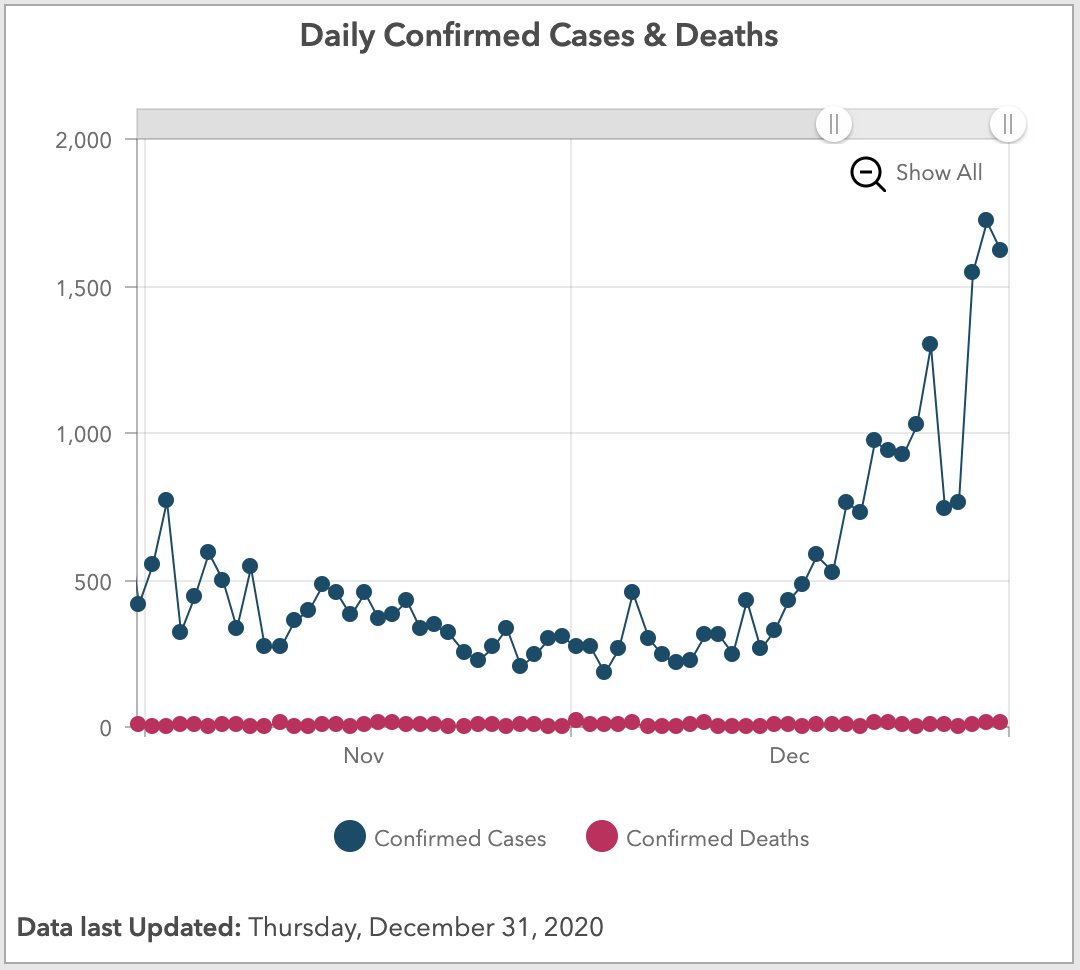
CodyyyGardner Categories Health
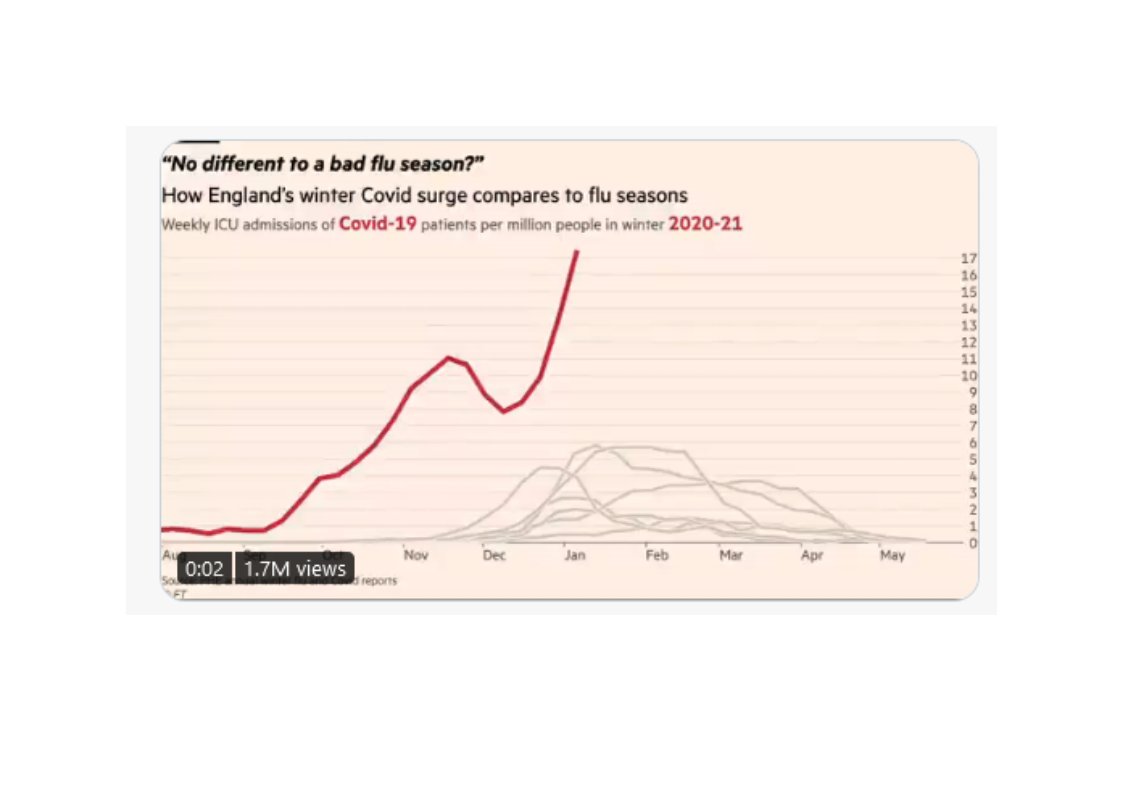
NEW: a common response to reports of hospitals struggling this winter is "it\u2019s no different to a bad flu season!"
— John Burn-Murdoch (@jburnmurdoch) January 7, 2021
I\u2019ve tracked down historical data on flu ICU admissions, including winter 2017-18, a record high.
Here\u2019s how England\u2019s Covid winter compares to a bad flu season \U0001f4f9 pic.twitter.com/tsExrDZM31
27/42 Some sceptics arguing covid-19 tests are inaccurate. PCR tests not 100% accurate but hospital inpatient testing accuracy much increased by frequency of testing (typically admission, days 3 & 6/7, then weekly). This means very low numbers of overall false positives.
28/42 Some sceptics argue that the published covid-19 positive inpatient numbers include both those admitted with covid-19 and those who acquired covid-19 in hospital. And that there are significant numbers of patients who have acquired covid-19 in hospital.
29/42 Covid-19 positive test data has always included anyone testing positive, irrespective of initial diagnosis. And the NHS has always acknowledged that hospital acquired (nosocomial) infection is a big issue. Hospitals are working incredibly hard to control it….
30/42 …The NHS regularly and completely transparently publishes nosocomial infection data, by hospital. But neither issue affects the degree of pressure that hospitals are under. Every inpatient, irrespective of initial diagnosis/infection source, occupies a hospital bed.
But TRASH "health" agencies & experts continue w/their Wear A Mask campaign & suppress niacin
Bacterial Pneumonia and Other Health Risks of Wearing Masks Alarm Doctors https://t.co/8eKmIaxeMQ
— Toni (@Landau_18901) January 3, 2021
https://t.co/1DRUO9L3ap
And remember, @CDCgov already concluded in systematic review of 14 RCTs that masks don't mitigate influenza spread, and a meta analysis further evidenced that even N95 masks make no difference vs cloth masks, meaning that no masks - not even N95 - workhttps://t.co/mSwdz7U6tM
— 3PIDEMIOLOGY (@3PIDEMIOLOGY) December 31, 2020
348,601 "ever-#snus users had about 60% lower Parkinson's disease risk compared with never-snus users."
https://t.co/YHB9FKkUtQ
30,000 British doctors followed for 60 years: "current smokers at baseline had a 30% lower risk of
#MedicalNicotine
Nicotine is beneficial for people with #ADHD. Research on adults and adolescents with ADHD shows that nicotine patches improve focus and attention, and reduce hyperactivity &
ADHD: "Nicotine ...may have properties similar to stimulant medications (e.g., Ritalin) used to treat ADHD. [It] may increase attention and reduce hyperactivity & impulsivity."https://t.co/l9QVnJHBhl#MedicalNicotine #ADHD #ADHDAwareness #Autism #Neurodiversity #Neurodivergent
— ClovisSangrail (@ClovisSangrail4) January 3, 2021
#MedicalNicotine
Nicotine reduces symptoms of Alzheimer's disease (AD).
https://t.co/Tht2Y8CZiN
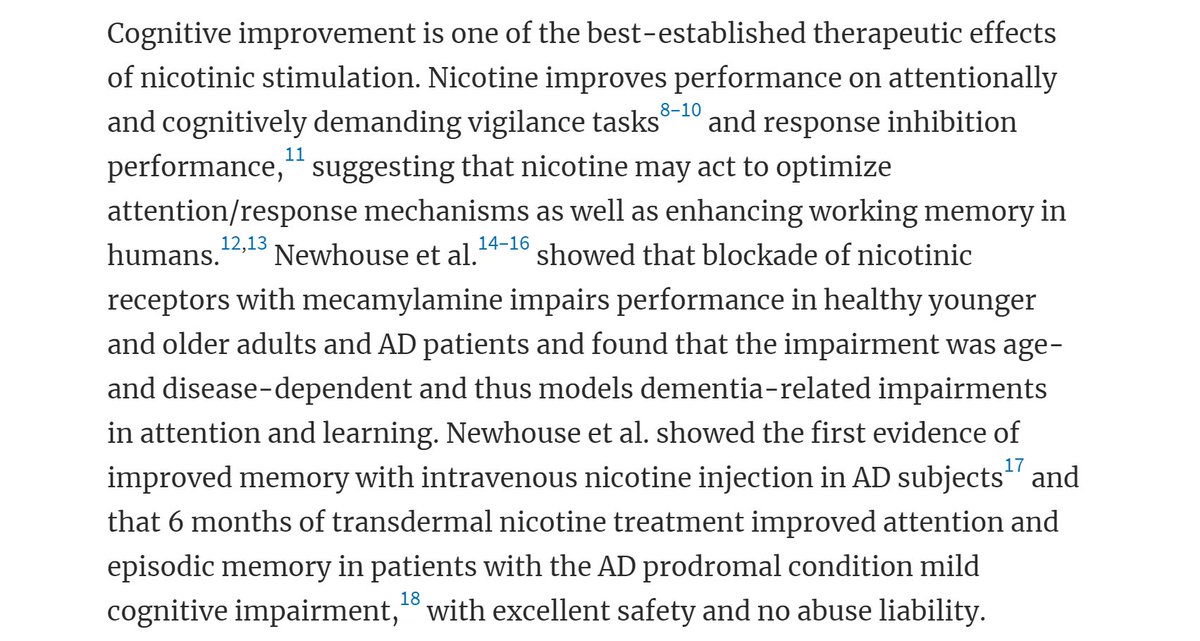
#MedicalNicotine
Nicotine is beneficial for people with schizophrenia. More than 70% of people with schizophrenia smoke.
#SaferNicotine alternatives could help them as therapy, and to not die from
#MedicalNicotine
Nicotine, "(either 2 mg nicotine gum or 7 mg transdermal nicotine patch) potentiates [enhances] the therapeutic properties of neuroleptics in treating Tourette's syndrome... A single patch may be effective for a variable number of
A well-balanced piece. Bed occupancy rate in NHS is actually lower than usual - even with fewer beds. (Though spare capacity has been created through cancellation of non-urgent operations etc, and higher levels of staff sickness are causing pressures.) https://t.co/CH8hGcFOs9
— Paul Embery (@PaulEmbery) January 8, 2021
Under normal circumstances, most NHS acute hospitals will have several types of inpatient areas
1. Assessment unit
2. Specialty wards
3. Intensive care
As well as outpatients, emergency department, day case surgery etc.
Patients admitted from A&E would go to 1, then move to 2. Some might go directly to 2, sickest ones to 3.
In many hospitals, the assessment unit is vital to flow of patients out of Emergency Department.
With COVID, several blocks have been introduced. Firstly patients have to be treated as "hot" in 2m apart bed spaces until their test results are back. This reduces an average six bedded bay to four.
There are rapid tests that turn around in around an hour or two, but their availability is limited. PCR still takes up to 24 hours to get back (often quicker), and lateral flow in the population admitted to hospital isn't sensitive enough to pick up silent cases.