As US hospitals make the necessary shuffle to accommodate the current wave, I would like to remind leadership about the study done on the psychological status of frontline hospital workers during NYC's spring Covid surge (thread).
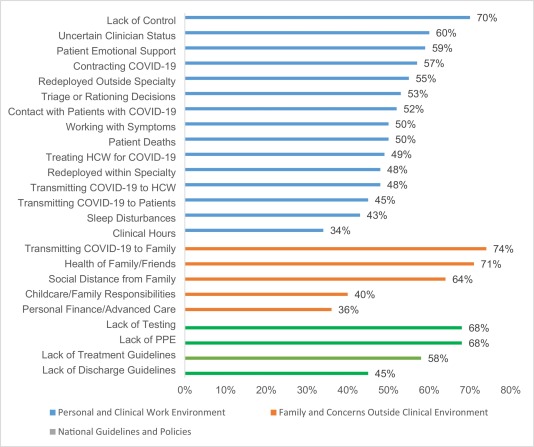
- Perceptions of a lack of control and/or uncertainty
- Performing clinical work that is outside of your specialty
- The need/expectation for healthcare providers to provide social support to patients in lieu of their families (due to visitation restrictions)
- And also fears related to getting/transmitting Covid within the work environment - in particular, the uncertain Covid status of other healthcare providers
More from Health
🚨Important changes to lockdown/self-isolation regulations from 5pm
The Health Protection (Coronavirus, Restrictions) (All Tiers and Self-Isolation) (England) (Amendment) Regulations 2021
£800 'house party' FPN & police can now access track & trace data
https://t.co/k9XCpVsXhC
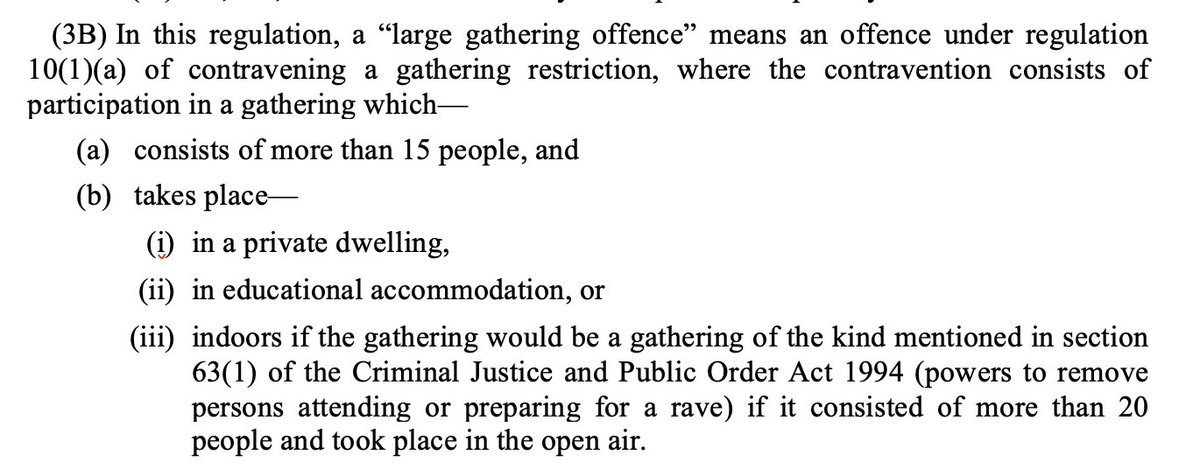
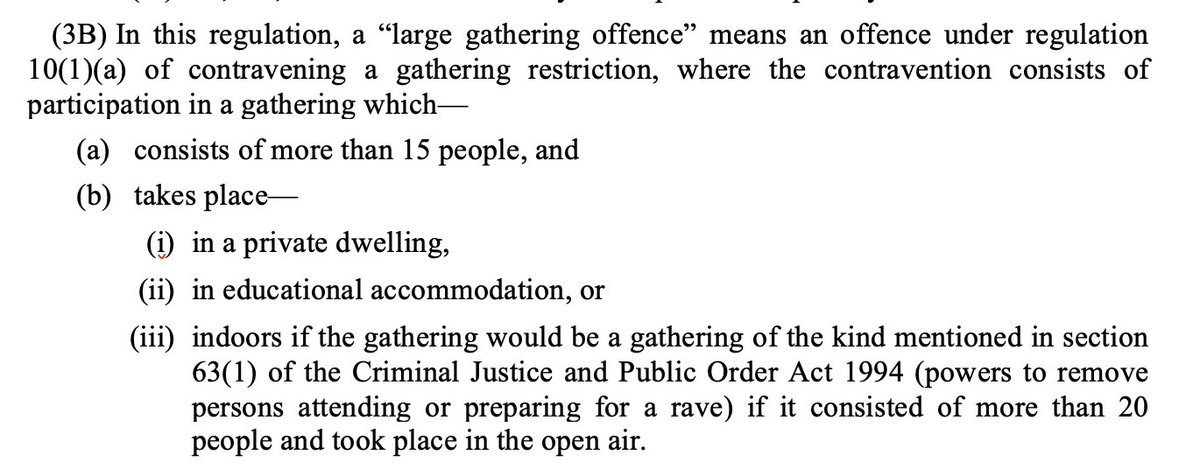
“Large gathering offence”
As trailed by Home Secretary last week there is now a fixed penalty notice of £800 (or £400 if you pay within 14 days) for participating in an gathering of over 15 people in a private residence
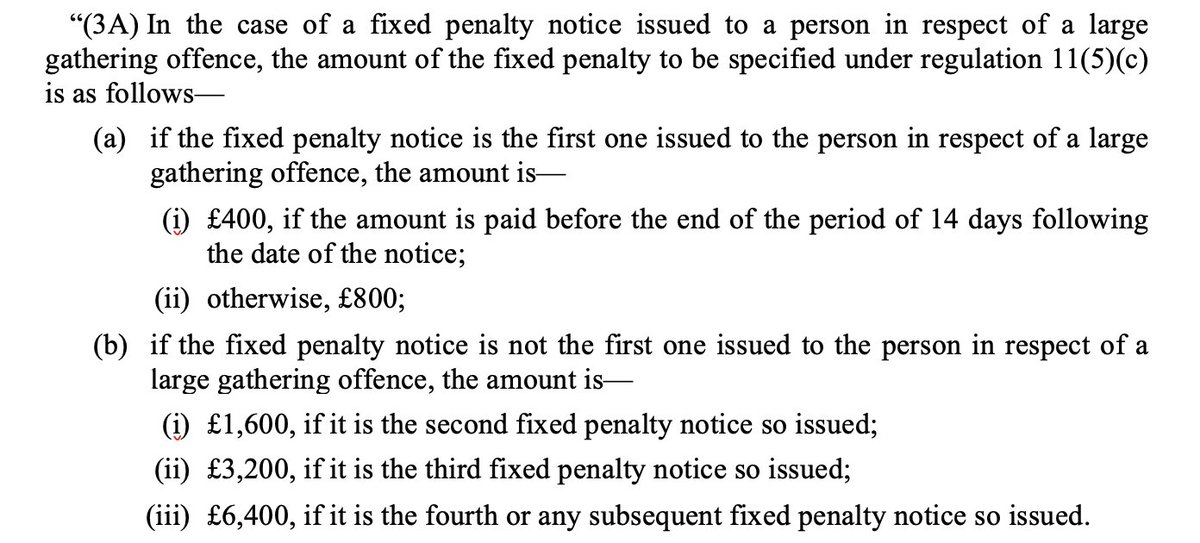
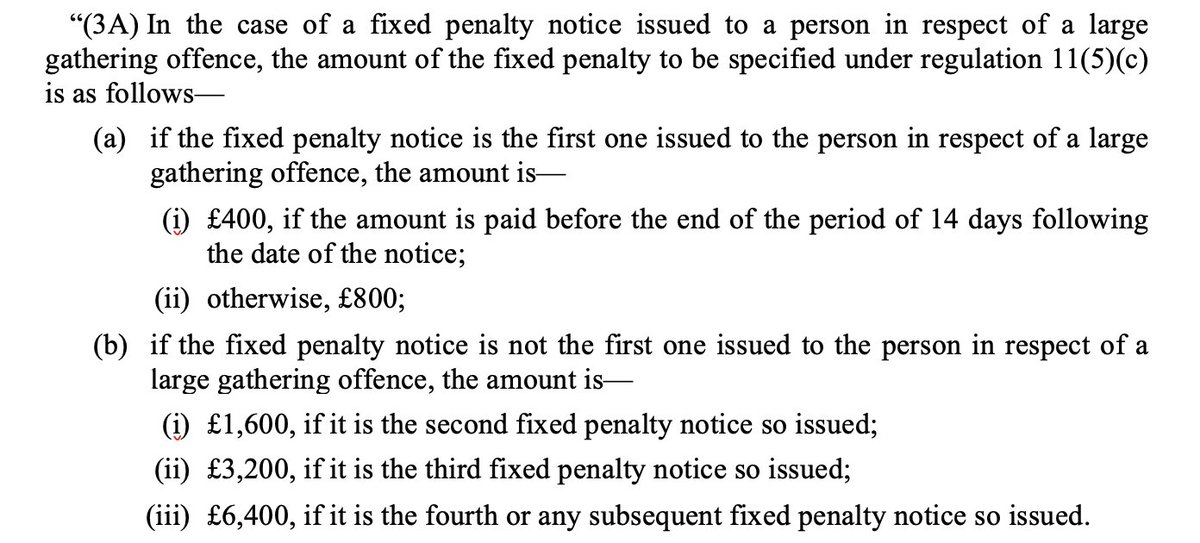
Fixed Penalty Notices double for each subsequent “large gathering offence” up to £6,400
Compare:
- Ordinary fixed penalty notice is £200 or £100 if paid in 14 days
- Holding or being involved in the holding of a gathering of over 30 people is £10,000
Second big change:
Since September has been a legal requirement to sell-isolate if you test positive/notified by Track & Trace of exposure to someone else who tested positive
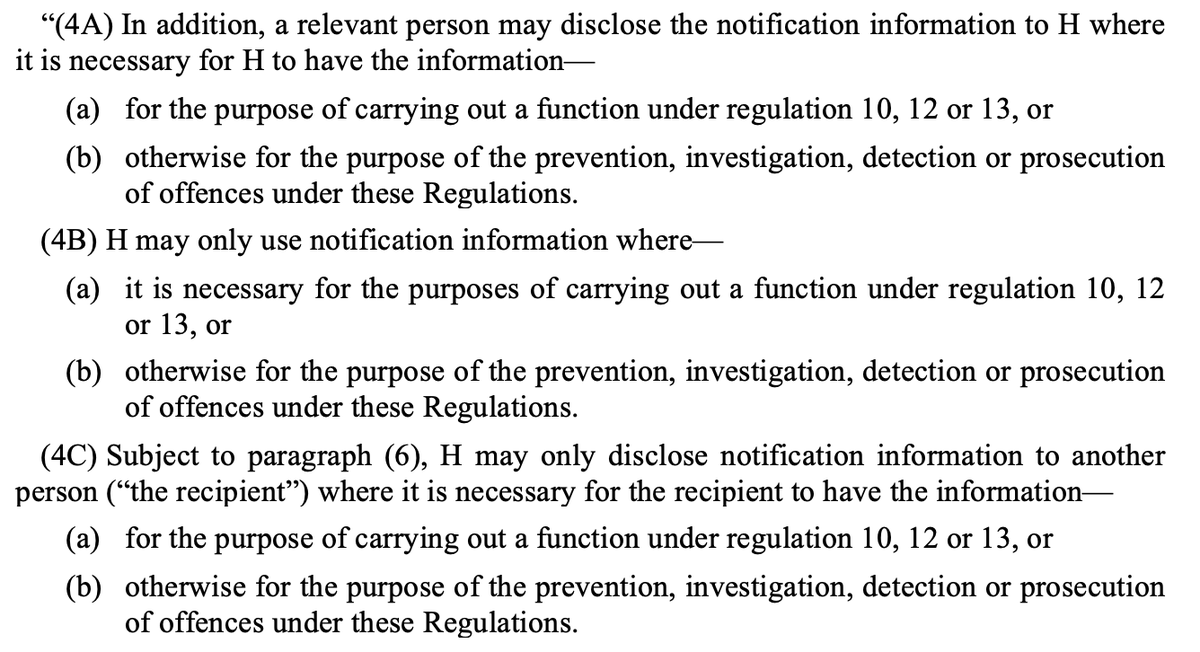
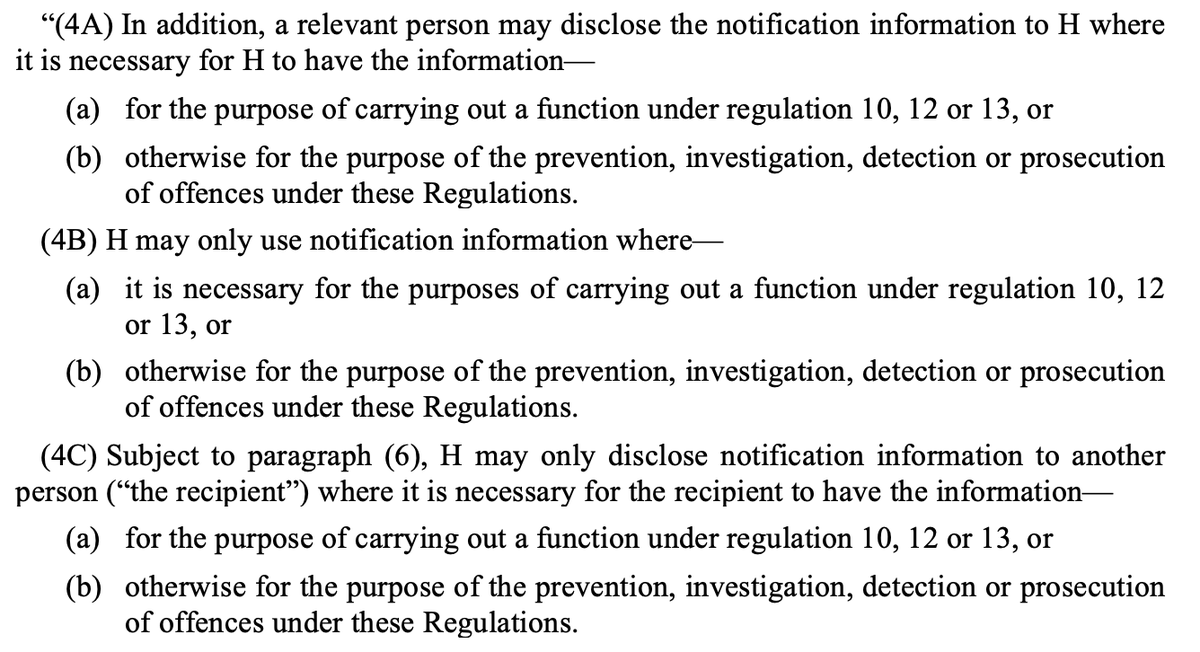
Police can now be given access to NHS Track & Trace data if for the purpose of enforcement/prosecution
This will make it easier for police to enforce people breaking self-isolation rules. Currently there has been practically no enforcement.
Data says only a small proportion of people meant to be self-isolating are fully doing so.
The Health Protection (Coronavirus, Restrictions) (All Tiers and Self-Isolation) (England) (Amendment) Regulations 2021
£800 'house party' FPN & police can now access track & trace data
https://t.co/k9XCpVsXhC
“Large gathering offence”
As trailed by Home Secretary last week there is now a fixed penalty notice of £800 (or £400 if you pay within 14 days) for participating in an gathering of over 15 people in a private residence
Fixed Penalty Notices double for each subsequent “large gathering offence” up to £6,400
Compare:
- Ordinary fixed penalty notice is £200 or £100 if paid in 14 days
- Holding or being involved in the holding of a gathering of over 30 people is £10,000
Second big change:
Since September has been a legal requirement to sell-isolate if you test positive/notified by Track & Trace of exposure to someone else who tested positive
Police can now be given access to NHS Track & Trace data if for the purpose of enforcement/prosecution
This will make it easier for police to enforce people breaking self-isolation rules. Currently there has been practically no enforcement.
Data says only a small proportion of people meant to be self-isolating are fully doing so.
Very important that obvious failures with Track and Trace and self-isolation (study late last year said 18% of people complying https://t.co/dhJUZ7Pm0l) are not painted as an enforcement issue. Plainly not. Would just pass buck to police who have almost no capacity to enforce https://t.co/Eb4Kl5Ze0E
— Adam Wagner (@AdamWagner1) January 25, 2021