Currently too often patients with high creatinine are given too much IV fluid, driven by an AKI ➡️ fluid reflex
We’ve seen 7 litres be given in one shift.
Medics & surgeons, juniors & seniors, it seems everyone loves to reach for extra IV fluid (especially if urine output poor)
Why does huge volume IV fluid ‘resuscitation’ consistently occur?
Lots of reasons, including FALSE beliefs:
🛑 IV fluid always “treats AKI”
🛑 Hypotension = hypovolaemia
🛑 Lactate >2 means fluid deficiency
🛑 Septic patients are very hypovolaemic
The rule with IV fluids and AKI is to remember this 5 word phrase:
💥 💥 Aim for euvolaemia, then stop💥 💥
Fluid status is like Goldilocks - hypovolaemia is bad for the kidneys BUT excess volume is also harmful for renal function and will cause other complications too.
It is easy to say “target euvolaemia” - but we agree it is more difficult to do!
Fluid status assessment is certainly made harder by a belief that we must only rely on a snapshot assessment of examination features which are NOT specific / sensitive / reliable to elicit like.…
🔹 Cool peripheries
🔹 Bibasal crackles - highly nonspecific in older patients!
🔹 Dry skin
🔹Tachycardia
🔹 x and y descent of the JVP wave…..
Even postural BP drop, one of the better performing signs for hypovolaemia, still has a wide differential diagnosis.
Serial physical examinations by one clinician improves assessment, but this is challenging given shift patterns.
And unfortunately the blood tests can be misleading too - for example check out our previous post about other causes of raised urea 👇
https://t.co/CSiRRnMi1a
TIP - things get better when the adage of ‘history trumps examination’ is observed:
1️⃣ Has there been volume loss?
2️⃣ Has there been decreased intake?
If the answer is “not really” to both of these, then think carefully about what you think more fluid will accomplish.
So….
When phoned as renal reg on-call on day 2-3 we’re usually not thinking “easy hypovolaemic AKI” but are concerned something is being missed.
Three common things:
1. AKI is part of sepsis / hypotension / MOF badness: patient needs ICU & vasopressors, not more IV fluid
2. AKI is intrinsic or post-renal: patient needs a diagnosis (think urinalysis, ultrasound, discussion), not more IV fluid
3. AKI is an additional signal that palliative care may be appropriate (remember stage 3 AKI has terrible 42% mortality at 30 days in patients >75 years)
Pre-renal AKI purely due to hypovolaemia generally improves fast.
If the patient has a great story for hypovolaemia but their creatinine is rising/stuck, then they often have a degree of acute tubular necrosis (ATN).
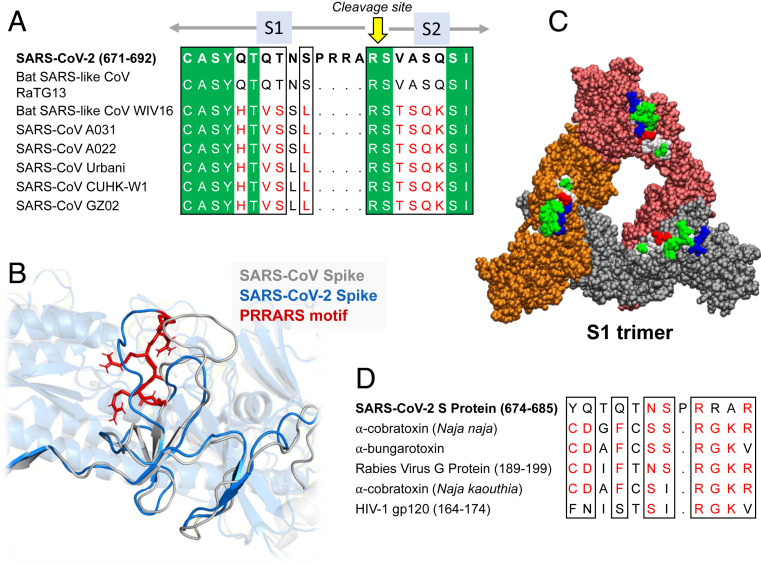
Let us show you something (it’s not as boring as it appears!)
On left is ATN with gaping spaces in tubules, & on right is healthy kidney with nice plump tubules.
Appreciate that there is actual histological change - this needs TIME to recover
✳️ Just as injured cells in stroke or MI don’t magically heal with IV saline, neither does ATN ✳️
✅ Sometimes you’ll get a patient with ATN to euvolaemia & they still won’t pee. That’s OK - not an indication for more fluids
✅ Remember low urine output is a warning you have less margin for error before causing hypervolaemia - again, shake off the reflex just to ⬆️fluid rate
“Are there exceptions?”
Not really - there’s different risk:benefit in different scenarios
👉 in tumour lysis, myeloma or rhabdo for example we do try to target higher urine outputs
BUT when patient is well-filled & not peeing much, we’re re-thinking rather than ploughing on.
“But does volume overload even matter?”
YES - and it’s not just the obvious pulmonary oedema badness.
Excess fluid ➡️ high venous pressure ➡️ decreased perfusion pressure for heart, brain, liver (& kidneys!!)
Patients with excess volume have:
🛑 longer AKI
🛑 higher mortality
In hypovolaemic AKI aim to stop fluids before complications develop - you do not need to “swell to get well”.
Avoidable dialysis for ⬆️volume continues because of myth that the hugely complex pathophysiology of AKI is easily remedied by IV salty water (pic from Ostermann et al)
So apologies for the rant. But we hope we have made you think about why:
🛑 “I can’t give fluid for their AKI because they are already overloaded” makes no sense 🛑
And why:
🛑 “I’ll keep giving IV fluids until their oxygen sats drop” is just bonkers 🛑
Take home points:
✅ Prescribe IV fluid with the care you would warfarin
✅ Achieve euvolaemia, then sit on your hands
✅ If urine output or BP stays low think “Is a different approach needed here?” rather than autoreaching for more IV fluid
✅ Break your AKI ➡️ fluid reflex
As ever all comments/disagreements very welcome - it’s a tricky topic to teach & not done really at med school, so we at
@BukuRenal (@jamiekwillows this time) appreciate any feedback.
Would love to hear views on how you approach teaching ward junior docs
@NephroGuy @icmteaching