New NHS reforms announced today. Seems to be a story of two parts, plus a missing character. Quick thoughts (1/):
https://t.co/GChxwuvEF4
https://t.co/0tYunQaWkz
https://t.co/bMB9vvZm8t
(12/12) @HealthFdn
More from Health
Thread on how atheism leads to mental retardation (backed with medical citations🧵💉)
To start with, atheism is an unnatural self-contradicting doctrine.
Medical terminology proves that human beings are naturally pre-disposed to believe in God. Oxford scientists assert that people are "born believers".
https://t.co/kE0Fi588yn
https://t.co/OqyXcGIMJn

It should be known that atheism could never produce an intelligently-functioning society and neither ever will.
Contrastingly, Islam produced several intellectuals & polymaths, was on the forefront of scientific development, boasting 100% literacy
It is also scientifically proven that atheism led to lesser scientific curiosity and scientific frauds, which is also why atheists incline to pseudo-science.
Whereas, religion in general and Islam in particular boosted education.
https://t.co/19Onc84u3g

Atheists are also likely to affected by pervasive mental and developmental disorders like high-functioning autism.
Cognitive Scientists and renowned Neurologists found that more atheism is leads to greater autism.
https://t.co/zRjEyFoX3P

To start with, atheism is an unnatural self-contradicting doctrine.
Medical terminology proves that human beings are naturally pre-disposed to believe in God. Oxford scientists assert that people are "born believers".
https://t.co/kE0Fi588yn
https://t.co/OqyXcGIMJn

It should be known that atheism could never produce an intelligently-functioning society and neither ever will.
Contrastingly, Islam produced several intellectuals & polymaths, was on the forefront of scientific development, boasting 100% literacy
If the Muslim world had not existed, there literally would be no technology/achievements today.
— Starks\u262a\ufe0f\U0001f1f9\U0001f1e9 (@MegaIntelIect) January 8, 2021
Science only developed because of Islam, Europe should be grateful to Islam for civilizing their barbaric cult.
Source: The Caliph's Splendor, Pg 204-05 https://t.co/HVypO52Tpc pic.twitter.com/00jYSbaDSs
It is also scientifically proven that atheism led to lesser scientific curiosity and scientific frauds, which is also why atheists incline to pseudo-science.
Whereas, religion in general and Islam in particular boosted education.
https://t.co/19Onc84u3g

Atheists are also likely to affected by pervasive mental and developmental disorders like high-functioning autism.
Cognitive Scientists and renowned Neurologists found that more atheism is leads to greater autism.
https://t.co/zRjEyFoX3P

You May Also Like
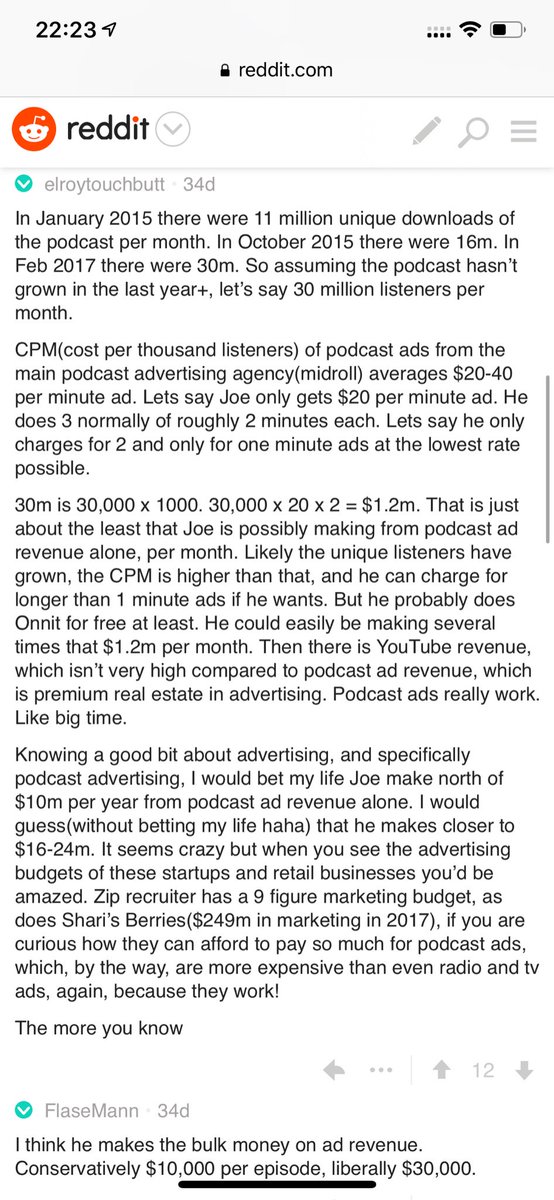
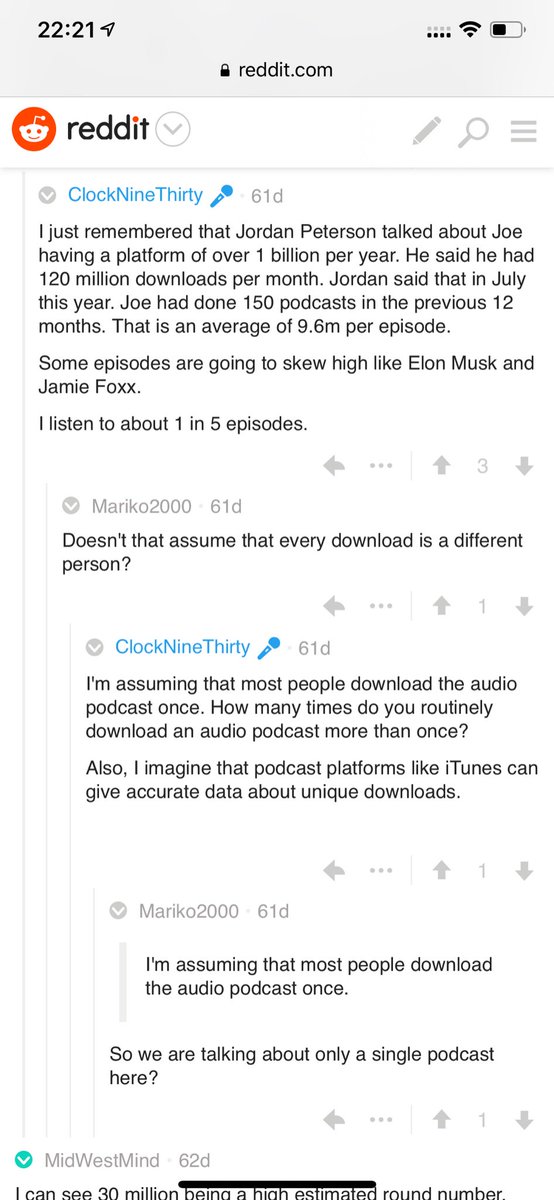
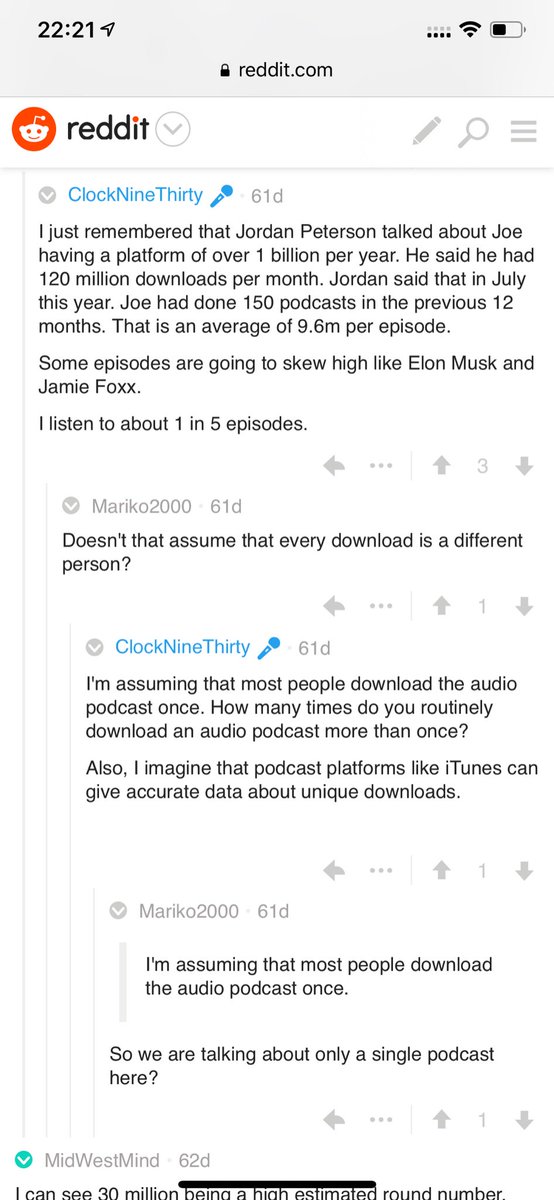
Joe Rogan's podcast is now is listened to 1.5+ billion times per year at around $50-100M/year revenue.
Independent and 100% owned by Joe, no networks, no middle men and a 100M+ people audience.
👏
https://t.co/RywAiBxA3s
Joe is the #1 / #2 podcast (depends per week) of all podcasts
120 million plays per month source https://t.co/k7L1LfDdcM
https://t.co/aGcYnVDpMu
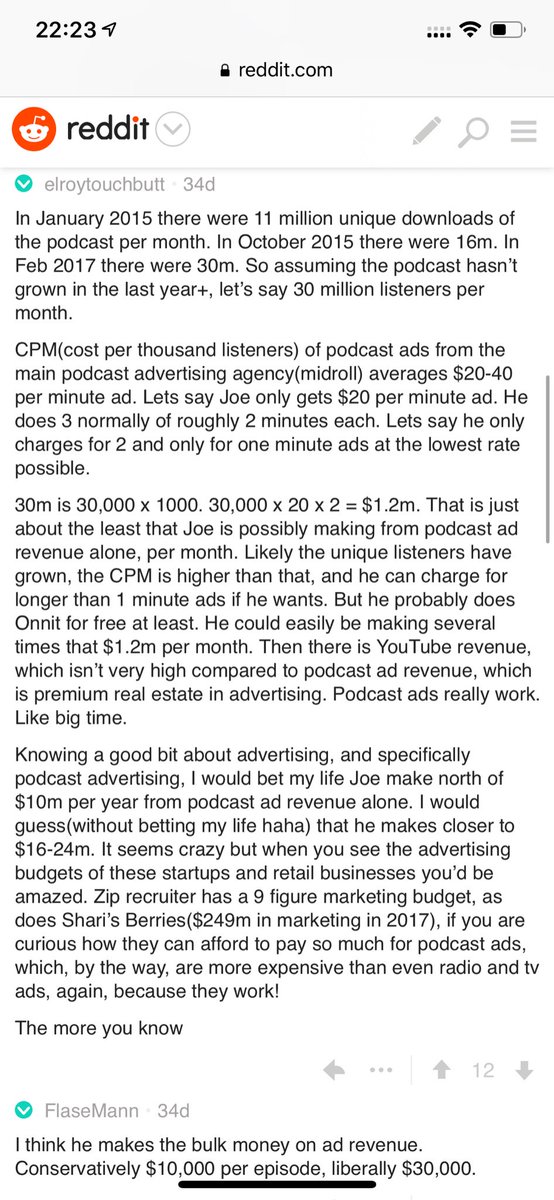
Independent and 100% owned by Joe, no networks, no middle men and a 100M+ people audience.
👏
https://t.co/RywAiBxA3s
Joe is the #1 / #2 podcast (depends per week) of all podcasts
120 million plays per month source https://t.co/k7L1LfDdcM
https://t.co/aGcYnVDpMu